FAQs
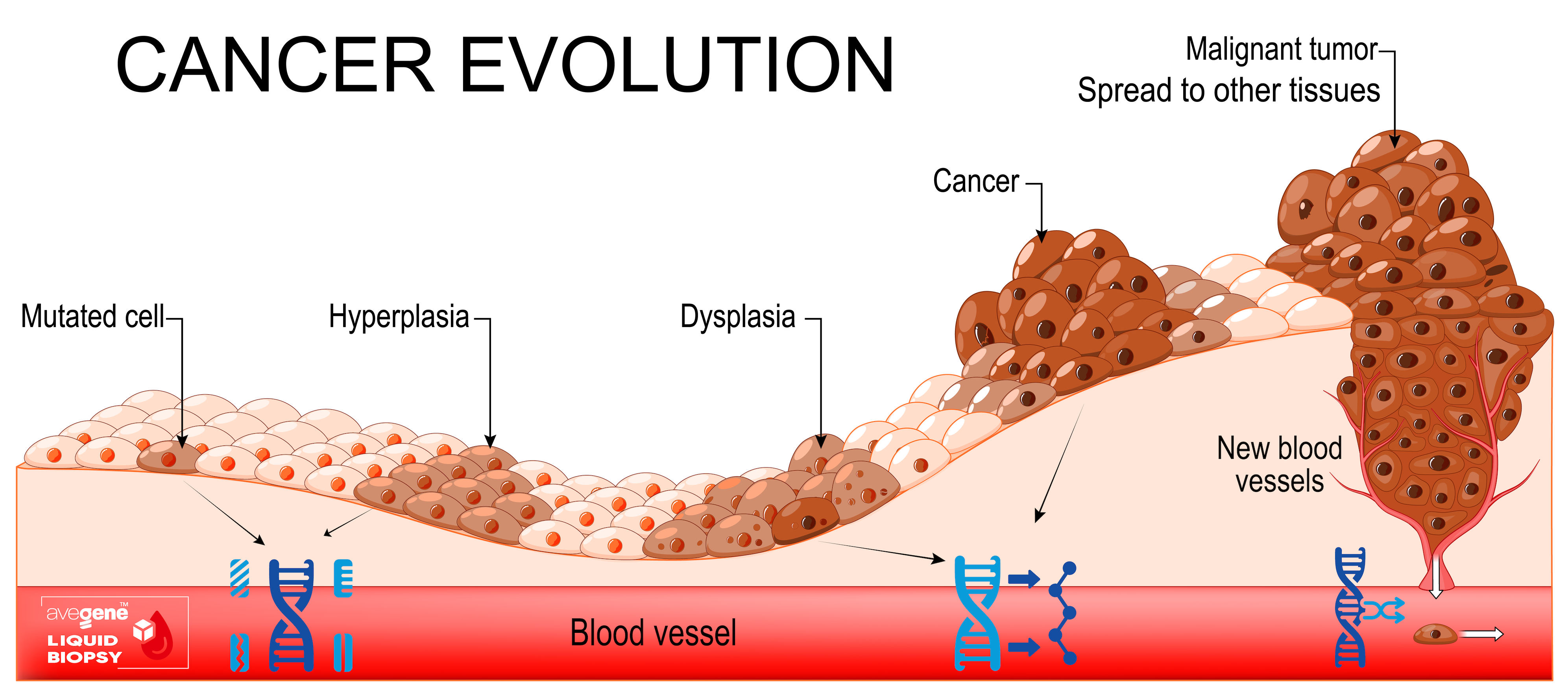
Cancer occurs when cells develop uncontrolled and spread. Any of the billions of cells in the human body can become cancer. Human cells normally divide to make new cells as needed. Old or damaged cells die, and new ones replace them. This ordered process might fail, causing aberrant or damaged cells to reproduce. Tumours can arise from these cells. Tumours can be malignant or benign. Cancerous tumours infiltrate neighbouring tissues and can metastasise to generate new tumours. Tumours can be cancerous. Benign tumours do not infect neighbouring tissues. Benign tumours seldom return, although malignant ones sometimes do. However, benign tumours can become enormous.
In many ways, cancer cells are not the same as healthy cells. As an example, cancer cells
* grow even when there aren't any signs telling them to. Cells that are healthy can only grow when they get signs like these.
*Do not pay attention to messages that usually tell cells to stop dividing or die (this is called apoptosis).
*spread to other parts of the body from nearby places. When normal cells meet other normal cells, they stop growing. Also, most normal cells don't move around the body. Tell the blood vessels to grow towards the tumours. These blood tubes bring oxygen and food to tumours and take away waste from tumours.
* Stay away from your defence system. The immune system usually gets rid of cells that are broken or not working right.
*make your defence system help cancer cells stay alive and grow. In this case, some cancer cells trick defence cells into keeping the tumour safe instead of fighting it.
* go through many changes in their chromosomes, like adding or removing parts of chromosomes. There are twice as many chromosomes in some cancer cells as there should be.
* need different kinds of food than normal cells do. Also, some cancer cells use nutrients in a different way than most other cells do to make energy.
This speeds up the growth of cancer cells. A lot of the time, these strange behaviours are so important for cancer cells that they can't live without them. Because of this, researchers have been able to create treatments that target the abnormal parts of cancer cells. As an example, some cancer treatments stop blood arteries from spreading towards tumours, which means the tumour doesn't get the nutrients it needs.
Technically "Cancer" is a genetic disease. To put it another way, changes to the genes that control how our cells work, especially how they grow and split, are what cause cancer. Changes in genes that lead to cancer can happen for instance as a result: - of defects that happen when cells grow. - presence of dangerous Oncogenic substances in the environment, like the chemicals in smoke, ultraviolet rays, heavy metals - Oncogenic viruses (typically HPV, HB, HIV, Herpes family) These all can damage DNA (RNA) and thus replication of cells into unwanted mutation. Cells with broken DNA are usually killed off by the body before they become dangerous. But as we age, our bodies become less able to do that. Part of the reason why cancer risk goes up with age is because of this. Certain cells may also be more sensitive on improper replication due to hereditary genes that came from our parents (ancestors in general, sometimes grand or grand grandparents ). We call this group "Germinal Mutations" and its detection will help us to understand to what particular mutations/cancers we may be more sensitive to. The DNA changes that cause cancer are different for each person. More changes will happen as the cancer continues to grow. Different cells in the same tumour may have different genetic changes. Therefore we examine each h gene for different mutation parameter.
Metastatic cancer refers to cancer that has migrated from its original location to another part of the body. Metastasis refers to the spread of cancer cells to different areas of the body. Metastatic cancer shares the same name and cell type as the underlying malignancy. For example, breast cancer that forms a metastatic tumour in the lung is classified as metastatic breast cancer rather than lung cancer.
The main goal of our NGS testing is to detect any cell mutation as early as possible to avoid Metastasis.
Nowadays medicine can truly make miracles and cure patients but the basic prerequisite is to start the therapy at an early stage.
You can access your medical records by logging into your patient portal on our website. If you haven't set up your account, please contact our support team to assist you with registration.
In most cases, a referral is not necessary to see our specialists. However, depending on your insurance provider, a referral may be required. We recommend checking with your insurance company or contacting our support team for assistance.
There is no danger to any of your private data on AveGene.
We make sure that even the internal testing is done in secret. In a way, we don't even need to know the patient's name. The molecular state of the blood or plasma sample sent to us is only interpreted with an anonymous sample ID. The person who has the activation card information is the only one who can see the results.
Blood sample 20ml
Patient with non-small cell lung cancer:
- Detected: EGFR L858R mutation, river mutation with VAF 12%.
- Recommended treatment: EGFR inhibitors (e.g., osimertinib).
- Monitoring after 3 months of treatment: the VAF decreased to 0.5%, indicating a good response.
- Monitoring after 6 months: mutation T790M detected (VAF 2%) = resistance, treatment change recommended.
Variant allele frequency (VAF): Indicates the percentage of ctDNA carrying a specific mutation in the sample. For example: A VAF of 2% means that 2% of all ctDNA fragments contain this mutation. Higher VAF usually indicates a greater tumor burden.
Types of mutations:
1- Driver mutations: Changes that support the growth and spread of the tumor (e.g., mutations in EGFR in lung cancer).
2- Passenger mutations: Secondary changes that do not have a direct impact on tumor growth.
3- Gene amplification: Increased number of copies of a specific gene (e.g., ERBB2 in breast cancer).
4- Gene fusion: The joining of parts of two different genes, which can lead to the formation of abnormal proteins that support tumor growth (e.g., ALK fusion in lung cancer).
We value your feedback. You can share your experience with us by filling out the feedback form available on our website or by contacting our patient relations team at [Phone Number].
As part of the AveGene screening, we focus solely on diagnosis by interpreting the molecular status of the sample and comparing it with the standard (healthy) reference genome. The result is practically a list of identified genetic changes. Each change is assigned to a specific gene and type of mutation (e.g., point mutation, deletion). The VAF and the clinical significance of the mutation (e.g., "pathogenic," "likely pathogenic") are also provided.
However, the results of NGS liquid biopsy can be used by the patient's doctor primarily for:
Targeted therapy
If the mutation is "actionable" – i.e., there is targeted treatment available for it – the results often include a list of recommended drugs or clinical trials where the patient could benefit from therapy. For example, EGFR mutations in lung cancer indicate sensitivity to EGFR inhibitors (gefitinib, osimertinib).
Monitoring treatment response
Dynamic changes in VAF can show how the tumor responds to treatment. A decrease in VAF after treatment indicates a positive response, while an increase in VAF may signal resistance or relapse.
Detection of resistance
NGS can detect new mutations that arise during treatment and lead to resistance. For example, the T790M mutation in the EGFR gene is known for resistance to the first generation of EGFR inhibitors.
AVEGENE screening tests are an auxiliary tool, not a diagnosis. Our role is to interpret the molecular status of the tested sample. For diagnosis, it is necessary to take into account the following aspects, which must always be assessed by the patient's doctor.
Clinical context:
The results of NGS liquid biopsy should always be interpreted in conjunction with clinical findings, imaging methods, and the overall condition of the patient.
Sensitivity and limitations:
Although the NGS method is highly sensitive, there are situations where it may not detect all mutations, especially if the ctDNA concentration is very low.
Dynamics of the tumor profile:
Tumor cells are genetically heterogeneous and can mutate during treatment. Repeated testing of liquid biopsies therefore helps to monitor changes over time.
There is a test results password being used to get into locked files on the AveGene Health Portal.
You are safe in two ways.
1) The "forgot password" button can be used to get your portal password back.
2) You need to use the password that came with the Sample Collection Kit on the registration card to open the test results files. To get this password back, you need to be checked out by our expert during a short Teams meeting. You will need information like your personal passwords that you used to pay (REMEMBER! WE WILL NEVER ASK YOUR FUL CREDIT CARD DETAILS !).
This face to face verification process is here for your privacy and eliminates automated attempts to crack your data.
The data belongs to you!
This is why we retain the data on a secured site accessible just with your secret password. Always at AveGene we keep the data under a unique code 100% anonymously. Without employing our encryption system, the data file is constantly guarded by a password and does not link to any particular individual even if someone would hypothetically access it.
You need to find out what kinds of genetic treatments your insurance may cover by calling them.
Genetic tests financial coverage are administered in different ways in each country, and we are not able to go into specifics.
If you plan to use insurance, please make sure you know the rules with that company before you buy our screening tests.
The Sample Collection Kit comes with a special folder and label stickers, as well as everything else you need to safely pack and wrap the samples.
Choose the sample collection spot that is closest to you. You can use any courrier service you're used to.
Alternatively, you can go to one of our partner centres to get your blood drawn and leave the sample there. The centre will take care of it themselves.
BLOOD:
For Blood collection, you need to visit any medical center, hospital, laboratory or Medical Doctor authorized to draw venal blood. You can also use one of our partner's collection centers.
Take the Sample Collection Kit with you - blood collection tubes are standard vacuum tubes but filled with a special stabilization fluid allowing blood stabilization for 2 weeks under room temperatures. (2-30C)
URINE:
Urine samples can be easily taken at home.